Acne Keloidalis Nuchae is a chronic skin disease characterized by enlarged tissue lesion growth on the back of the neck, starting as small acne-like bumps which eventually fuse together into a singular mass. Surgical removal is usually recommended, especially if the patient’s condition does not improve with medication or laser treatment. Primary excision and closure is a conventional technique that is employed for AKN removal surgery. An advanced derivative of this basic method is known as Trichophytic excision and wound closure. It is performed in such a way that allows hair to grow through the resulting scar tissue to avoid forming a line of emptiness, producing a better cosmetic outcome for the patient. According to Dr.U, a foremost leader and authority in the surgical treatment of AKN, Acne Keloidalis Nuchae removal with trichophytic excision and closure are best recommended for certain patients who meet very specific selection criteria.
The Journal of the American Academy of Dermatology (JAAD) published Dr.U’s case study report, entitled, A Patient Selection Criteria and Innovative Techniques For Improving Outcome and Cosmesis in AKN Lesion Excision and Primary Closure this groundbreaking publication details a patient selection criteria developed by Dr.U for the application of the Trichophytic excision and closure technique, as well as three specific cases which illustrate the significantly improved cosmetic outcome which can result for qualified individuals who are eligible for this type of surgery.
The Trichophytic Technique As An Advancement In Primary Surgical Excision for Acne Keloidalis Nuchae Removal Surgery
Primary excision involves surgically removing a specific area of unwanted skin, in this case, an elliptical region affected by AKN lesional growth.
Within this methodology, Dr.U applies an electrosurgical tip (which cuts the skin tissue and coagulates blood vessels) to perform trichophytic excision in order to cut the superior (i.e. top) edge of the wound and the inferior (i.e. bottom) portion of the ellipse at very specific angles which compliment each other. His recommendation is that Acne Keloidalis Nuchae removal with trichophytic excision and closure is only applied for certain patients with a vertical lesional width of 3cm or smaller that is located in the upper nuchal area.
This technique is derived from strip surgery hair transplantation, where a narrow strip-like section on the back of the patient’s scalp is removed as a source of donor hair follicle grafts which are harvested and then implanted into the hair loss regions.
The superior wound margin which is located at the top of the ellipse is cut at a slant that is parallel to the hair angles, producing a beveled and inverted wound edge.
Dr. U also shaves a 2-4 mm margin of skin around the inferior wound edge which removes the top part of the hair follicles embedded at the superficial dermal level.
Trichophytic Wound Closure for Acne Keloidalis Removal Surgery
In the two-layered trichophytic closure step ( which follows the trichophytic elliptical excision of the AKN lesion) the superior wound margin edge is pulled to cover and oppose the shaved skin margin around the inferior wound edge which contains the decapitated hair follicles.
Cases of smaller vertical excision widths (e.g. 2.5cm) may have the wound edges sutured together within the same surgery. A generously thick layer of bacitracin ointment is then applied to cover the wound. Typically, sutures can be removed around 7 days following the procedure but will vary for specific patients.
Otherwise, for patients with wider vertical excisions who also qualify for trichophytic excision and closure, Dr.U recommends using tension sutures, allowing the wound to gradually close on its own.
Dr.U’s Patient Selection Criteria For Bump Removal- Who Qualifies for Acne Keloidalis Nuchae Removal With Trichophytic Excision and Closure
As noted earlier, Dr.U introduced to the medical field of AKN treatment, the concept of defining patient screening criteria to select individuals eligible for Acne Keloidalis Nuchae removal with trichophytic excision and closure surgical techniques.
Prior to the publication of this new insight, no such qualifying system has been in place. AKN surgical practitioners would apply one of two approaches for patients:
- Primary closure and healing by primary intention
- Secondary closure and healing by secondary intention
Selection of either technique was often subject of arbitrary debate with the lack of an objective, well-defined set of criteria. Dr.U believes this explains the phenomenon where patients would receive one or the other with a fraction of them reporting poor cosmetic results or recurrence of the AKN.
Acne Keloidalis Nuchae Patients Who Qualify for Trichophytic Excision and Wound Closure
In his JAAD publication, Dr.U proposes specific selection criteria for choosing individuals for Acne Keloidalis Nuchae removal with trichophytic excision and closure. The intent would be to remove the lesions and close the wound so that hair ends up growing through the scar tissue.
The qualifying factors for this approach include AKN lesions that are 3cm or less in vertical width and located in the upper nuchal area.
AKN lesions which are present in the upper half of the nuchal area are closer to the occipital protuberance, or the fulcrum, which is the highest point of the skull’s curvature (on the back of the head). In this particular location, there is a reduced risk of scar stretching compared to the lower regions of the nuchal area which is more subject to the moving forces of the neck.
Also, according to Dr.U, AKN lesions which are less than or equal to 3cm in vertical width are at less risk for experiencing sudden dehiscing forces which can break the wound open. This is why they are suitable for Acne Keloidalis Nuchae removal with trichophytic excision and closure.
Immediate Versus Gradual AKN Wound Closure
For eligible patients who qualify for Acne Keloidalis Nuchae removal with trichophytic excision and closure, Dr.U specifies that wounds with a smaller vertical width (e.g. 2.5cm) can be closed on the same day, at the end of the surgical procedure.
Furthermore, wounds approximating closer to 3.0cm can be allowed to close gradually on their own with the aid of tension sutures. The purpose of applying tensional forces is to increase resistance within the tissue surrounding the wounds.
Gauze pad bolsters are used to minimize the pressure of the suture wires against the skin, preventing them from cutting through.
Within the first 48 hours, this will cause fibroblasts to differentiate into myofibroblasts cells which guides the process of wound contraction in the right direction.
According to Dr.U, the use of tension sutures will diminish the need for patients to constantly keep their head up in order to prevent the wound from stretching. Another benefit of their application is producing much thinner scars.
Three Acne Keloidalis Nuchae Real-Life Patient Examples By Dr. U Which Illustrate the Use of Effective Selection Criteria and Trichophytic Excision and Wound Closure Techniques
In Dr. U’s published JAAD article on AKN patient selection and the usage of trichophytic surgical methods, three real-life patient cases are discussed which illustrate the methods used for their procedures and the quality of their long term healing outcomes.
Within all three instances, the Acne Keloidalis Nuchae tissue targeted for removal was present in the upper part of the nuchal area.
The first patient mentioned was a 49-year-old male of African descent with an AKN lesion smaller than 2.5cm in vertical width. He qualified for immediate trichophytic closure of the wound during his procedure, where the sutures were removed 7 days after his surgery.
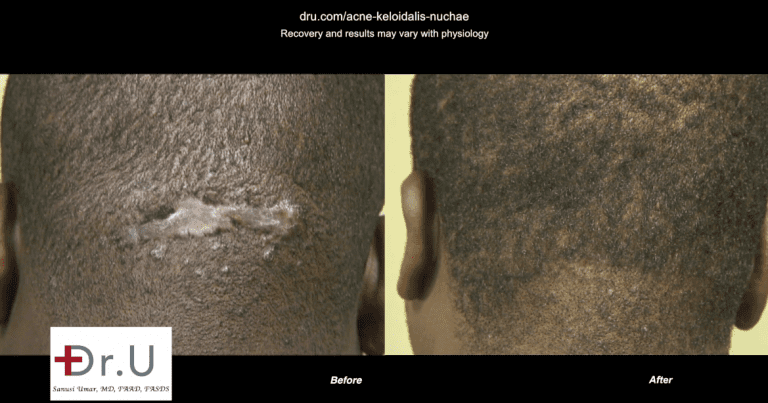
A one year follow up showed that his scar continued to be well concealed due to the hair growth through it. At this point, there was no sign of scar stretching or recurrence of the AKN tissue.
The second patient of the publication was an African American male who was 48 years of age. He presented a three-year history of his Acne Keloidalis Nuchae condition with pain and drainage due to lesional plaque that measured 3cm in vertical width, with overall dimensions measured at 4x3x1cm. Treatment with an oral antibiotic and intralesional steroids failed to improve his condition.
Dr.U applied his Acne Keloidalis Nuchae removal with trichophytic excision and closure along with the use of tension sutures (due to the 3cm width of the lesion) and gauze pad bolsters. No intraoperative complications were reported. Mupirocine 2% ointment was used throughout his post-operative treatment to prevent bacterial infection during the time that the wound is expected to gradually close on its own. The patient was also given the instruction to soak his bolster sutures on a daily basis with betadine solution.
At four weeks following the surgical excision, the tension sutures were no longer taut and could then be removed. No recurrence was noticed at this time.
Another follow up was performed at 14 months where the patient’s scar was observed s being thin and excellently camouflaged by the patient’s own hair growth.
The third patient mentioned in this report was a 46-year-old African American male. HIs AKN plaque had the dimensions of 6.5x3x0.5cm. Likewise, due to the vertical width being 3cm, Dr.U also applied tension sutures to this case in the same manner as patient 2, discussed above. His sutures were removed at just 2 weeks, at which time they lost their tautness. His scar was observed as being stable well-camouflaged with hair growth, along with a minimal degree of stretch.
These three reported patient cases all demonstrated excellent healing cosmesis along with no return of the Acne Keloidalis Nuchae tissue growth.
Dr. U recommends and practices a different set of surgical treatment approaches, other than trichophytic excision and closure for patients with AKN lesions greater than 3cm vertically wide and/or present in the lower nuchal area. With the application of more specific diagnostic criteria for various manifestations of Acne Keloidalis Nuchae and matching individuals with relevant surgical methods, patients can universally experience more satisfactory cosmetic healing outcomes, with the risk of recurrence being rendered virtually obsolete.
Frequently Asked Questions – Acne Keloidalis Nuchae Removal With Trichophytic Excision and Closure
Will laser treatment help me get rid of Acne Keloidalis Nuchae for good? Or is it really necessary to undergo trichophytic surgery to completely remove the bumps on the back of my head?
The purpose of using laser energy is to epilate and remove ingrown hair shafts which promote the immune system responses that inflame the hair follicles and subsequently create the unwanted AKN lesional growth to occur. In some early stage cases, this may be a helpful form of treatment. But in others, this approach may not be effective. If laser does not improve your condition, then surgery would be recommended to remove the AKN tissue mass. The trichophytic methods discussed above would only apply if your AKN bumps have merged into a single plaque that is 3cm or smaller in vertical width and present in the upper portion of the nuchal area.
What do AKN medications do as far as treating the condition? Is it possible to experience the complete and permanent elimination of Acne Keloidalis Nuchae through the use of these drugs?
AKN medications include intralesional steroids and antibiotics. The steroids are injected into the tissue to help minimize the extent of inflammation. But they cannot stop this reaction from occurring or eliminate the AKN growth altogether. The antibiotics are used to kill the bacteria microorganisms which proliferate in the moist drainage of the AKN issue and also contribute to the immune system inflammatory attacks. In rare cases, medications may help flatten small lesions and prevent them from worsening. But for most patients, they only reduce the symptoms of this condition (e.g. itching, pain and inflammation)
What happens if the AKN lesion is much lower and not located in the upper nuchal region? Is trichophytic excision still used?
For these cases, Dr.U recommends a different type of surgical excisional technique (i.e. not Acne Keloidalis Nuchae removal with trichophytic excision and closure) that would cause the wound to close into a linear scar that is aligned with the posterior hairline so that it is discrete and less noticeable.