UPDATE: While sclerotherapy and vein stripping (surgical varicose removal) are well-known treatments for varicose veins, they’re not for everyone because of their invasive nature. Laser leg vein removal is non-invasive and eliminates potential complications like bruising, bleeding, and discolorations, among other things, which, while non-common, can still be experienced with surgical removal and sclerotherapy.
Article Updated 2022
Dr. U Leg Vein Removal Services in Manhattan Beach, Los Angeles: The National Institutes of Health says that 60% of men and women suffer from some sort of vein disorder. Leg vein removal treatment has become increasingly popular with both men and women. Twenty-five percent of varicose vein sufferers tend to be men, although it is noted that it is almost always women who seek to remove veins in their legs.
What are Varicose Veins?
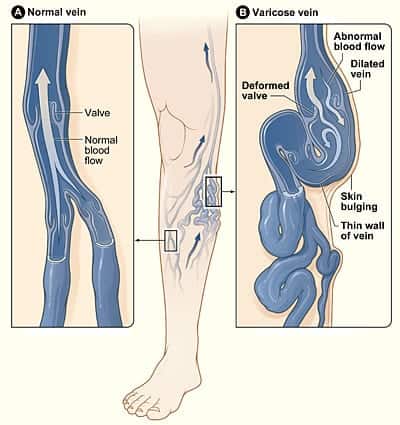
Varicose veins are gnarled, enlarged veins. Any vein can potentially become varicose, but the veins most commonly affected are found in the feet and legs. This is due to excessive standing and walking, which increases the pressure in the veins in your lower body. Plenty of people suffer from varicose veins or a more common and mild form called spider veins. Unfortunately, with the higher level of severity also comes additional effects of aches, pain, and discomfort. Varicose veins can even lead to more serious problems, such as blood clotting.
What Causes Varicose Veins?
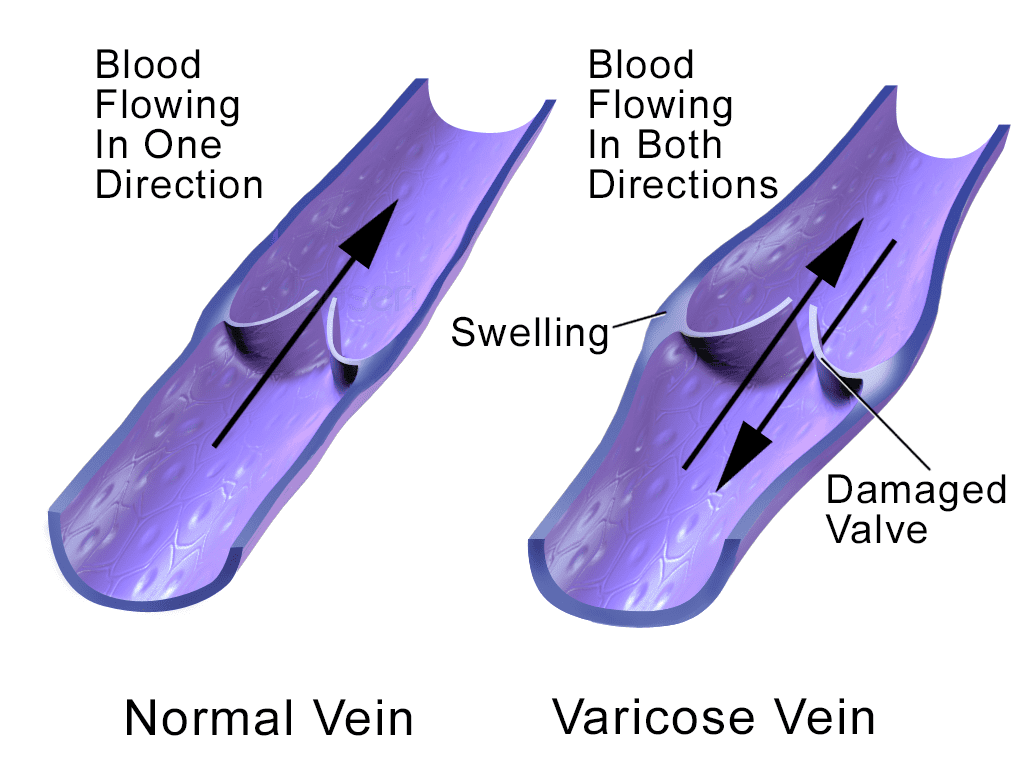
Varicose and spider veins can happen when valves designed to keep blood going to and from the heart and back down to the leg fail or become loose, causing there to be backwash, which can stretch the veins and slow leaking into the ankles and leg tissue, making it swell. Muscle contractions in the lower legs are used like pumps. The elastic vein walls contribute to blood returning to the heart. Small valves in the veins open up when blood flows toward the heart, and then they close to stop blood from flowing backward.
Causes of varicose veins can include:
- GENETICS: Genetic predisposition is the most important cause of varicose veins. A family history of varicose veins hints at a genetic predisposition, and offspring from the affected family are more likely than those from other families with no such history to develop them. The following factors can dictate varicose veins’ severity and onset time.
- AGE: As people age, their veins tend to lose elasticity, making them stretch. The valves in the veins can sometimes get weak, causing the blood that should be moving toward the heart to flow backward. Blood gathers in the veins, and the veins become enlarged and are considered varicose veins. The veins are blue because they contain deoxygenated blood recirculated through the lungs.
- GENDER: Varicose veins occur more often in women than in men. This may be because of a combination of activity, muscle tone level, and hormonal activity. Female hormones, estrogen, and progesterone, favor vessel relaxation and distensibility.
- PREGNANCY: Pregnant women may get varicose veins. Pregnancy increases the volume of blood in the body and decreases blood flow in the leg and pelvis. This circulatory change is meant to help the growing baby, but it may also produce an unsightly side effect — enlarged veins in your legs. Varicose veins can sometimes appear during pregnancy for the first time or get worse during late pregnancy due to the fact that the uterus puts greater pressure on the veins in the legs. The changes in hormones (increase in progesterone and estrogen) during pregnancy can also play a role. Varicose veins that appear at the time of pregnancy typically improve without medical treatment three to twelve months after delivery.
Types of Varicose Veins
There are multiple types of varicose veins, such as:
- Trunk varicose veins – These are near the surface of the skin and are thick and knobbly; they tend to be visible, usually long, and may look unsightly.
- Reticular varicose veins are red and often in close groups or networks.
- Telangiectasia varicose veins—These are also called thread veins or spider veins. They are small groups of blue or red veins that may be present on the face or legs. Unlike trunk varicose veins, they’re not harmful and don’t have a bulge underneath the skin’s surface.

Symptoms From Painful Leg Veins
Some painful signs and symptoms of varicose veins may include:
- An achy or heavy feeling in your legs
- Burning, swelling, throbbing, or muscle cramping in lower legs
- More aching in the legs after sitting or standing for a long time
- Itching surrounding one or more of your veins
- Bleeding from vein
- Discoloration in the skin and a painful cord in the vein
- Color differences, hardening of veins, inflammation in the skin, and ulcers near the ankle can mean a serious form of vascular disease that is in need of medical attention.
If you have a question about leg vein removal treatment, do not hesitate to Ask Dr. U at no cost using the consultation button below:
Preventing Varicose Veins
Most patients’ major cause of varicose and spider veins is hereditary. Some conservative methods can help reduce the symptoms of varicose veins and spider veins, but these methods do not prevent the progression of your venous disease. In order to prevent the need for leg vein removal, try not to stand or sit for long periods of time. Move around every 30 minutes. Take breaks throughout the day, putting the legs on a pillow when resting in order to ease discomfort. In addition, regular exercise helps to improve circulation and fend off varicose veins.
How to Remove Veins in Legs: Removal Methods
There are various methods for leg vein removal, including:
- Sclerotherapy
- External laser treatment
- Endovenous treatment using laser or radiofrequency
- Surgical removal
SCLEROTHERAPY: Dr. U recommends this leg vein removal method for 3mm or more in caliber veins. Various sclerosants (Injected chemicals) are available for this purpose. The doctor uses fine caliber needles mounted on syringes containing the sclerosant to inject into the vein and destroy it. Pressure stockings are often necessary after the treatment. It is fraught with possible complications, especially in cases where the veins are very small, and the sclerosant extravasates into surrounding tissue, causing severe bruising and tissue destruction to result in ulcers that could be disfiguring. Dr. Umar uses only FDA-approved sclerosants to remove veins in the legs and is an expert in injecting fine veins.
EXTERNAL LASER TREATMENT: External leg vein removal lasers are used right under the surface of the skin. This treatment may treat spider and tiny varicose veins just outside the skin. Typically, more than one leg vein removal session is needed. As your doctor prescribes, they are usually scheduled every 6 to 12 weeks. Walking is okay to do after treatment, and recovery is usually short. You’ll likely be able to return to your normal daily routine right after the leg vein removal laser treatment.
ENDOVENOUS ABLATION BY LASER AND RADIOFREQUENCY: Through this method of leg vein removal, the vein is cannulated with a fiber optic cord, which is done with sonographic or other monitoring processes for guidance. The cord is also equipped with a laser, radiofrequency, or other ablative processes that are discharged to destroy the veins as the cord is withdrawn. The method is useful in truncal veins that have complications like severe chronic nonhealing ulcers and debilitating vascular dermatitis. This method is usually done in centers that are dedicated to leg vein removal.
SURGICAL REMOVAL: This is indicated in truncal varicose veins with complications like chronic debilitating ulcers and dermatitis. Surgical leg vein removal entails surgical removal using techniques like vein stripping. However, it is becoming less appealing due to the advent of less invasive methods like endovenous ablation.
In 2002, Dr. Umar and colleagues did a laser leg vein removal study in the premier journal of dermatology (Dermatologic Surgery). This study compared three different laser categories typically used in leg vein removal. Not considering the names that are given to these lasers by the manufacturer, leg vein treatment lasers are in one of three categories:
1064nm (Nd YAG)
810 (Diode)
755nm (Alexandrite)
The study conducted by Dr. Umar and his colleagues showed that the Nd Yag (1064nm) laser was much superior to the others. [Blackwell Synergy – Dermatol Surg, Volume 28 Issue 3 Page 224-230, March 2002 (Article Abstract)]
Treatment Process and Recovery
The average time for laser leg vein removal is anywhere from half an hour to two hours in total. The time depends on each individual’s needs. Many patients worry that leg vein removal will affect their circulation; however, the blood will typically find other routes to circulate. Thanks to the use of a local anesthetic, there is minimal pain during the laser vein removal process. As no heavy medication is used, you are able to drive yourself to and from the office after leg vein removal treatment. Following the procedure, you can soon return to your normal activities.
Walking is encouraged, even on the day of treatment. While there may be slight discomfort, you are able to use over-the-counter pain medication such as ibuprofen or Tylenol to ease the discomfort. Occasionally, a patient will require stronger pain medication for a few days. Dr. U recommends wearing graduated compression stockings for the first two weeks after your procedure, which helps to provide support for healing and reduce pain. You may experience some bruising, soreness, and tenderness at treatment sites. There may also be a tightening sensation in your leg or a pulling sensation about two weeks into your healing process as your treated vein shrinks and begins reabsorbing into the body.
Leg Vein Removal Before and After Services by Dr. U Skin Clinic in Los Angeles

This Los Angeles patient turned to Dr. U for laser leg vein removal.

Beginning with many visible veins in the thighs, Dr. Umar successfully removed veins in the legs.
Dr. Umar Explains Treatment Options for Leg Veins:
Leg Vein Removal Services FAQ
When is leg vein removal surgery necessary?
Every patient’s case will be different, but leg vein removal surgery is generally suggested for patients with larger leg veins that won’t see much results from laser or other treatments. It’s also recommended if branches of blood vessels are giving the vein blood.
Can leg vein removal help with recurring veins if I’ve had my varicose veins stripped in the past?
Yes. If you notice that the veins are reappearing, consult Dr. U to determine the cause. In some patients, the veins will reappear and are often not well-functioning.
Can not removing an unwanted leg vein be harmful to my health?
Leg vein removal is normally for cosmetic purposes. However, in some cases, the leg vein can form hazardous conditions like blood clots or tissue breaking. A doctor can usually alert you to any health problems your leg vein may have.
Is the laser leg vein removal treatment dangerous?
Typically, complications related to varicose vein treatment are rare. Following the procedure, minor complications may include temporary discomfort, bruising, swelling, or discoloration. If you are facing these problems, Dr. U Skin Clinic recommends reaching out to your physician.
Are there varicose vein natural treatment options?
Although natural and at-home treatments will not have the best results for those already facing varicose veins, the methods below are great for prevention and the first signs of spider veins.
- Exercise
- Maintaining a healthy weight
- Essential oils
- An anti-inflammatory diet
- Herbs
Have more questions for Dr. U? Ask them using the button below.
Further Reading:
Learn more about removing unwanted moles from the face and body.
Read about how to prevent and treat stretch marks.
References
- Eremia S, Li C, Umar SH. A side-by-side comparative study of 1064 nm Nd:YAG, 810 nm diode and 755 nm alexandrite lasers for treatment of 0.3-3 mm leg veins. Dermatol Surg. 2002;28(3):224-230. doi:10.1046/j.1524-4725.2002.01162.x
- Sclerotherapy: Treatment for Varicose and Spider Veins. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/6763-sclerotherapy. Published 2022. Accessed August 2, 2022.
Removal Treatments of leg vein through images are quite systematically explained and the post is very easy to understand. Thanks for sharing.