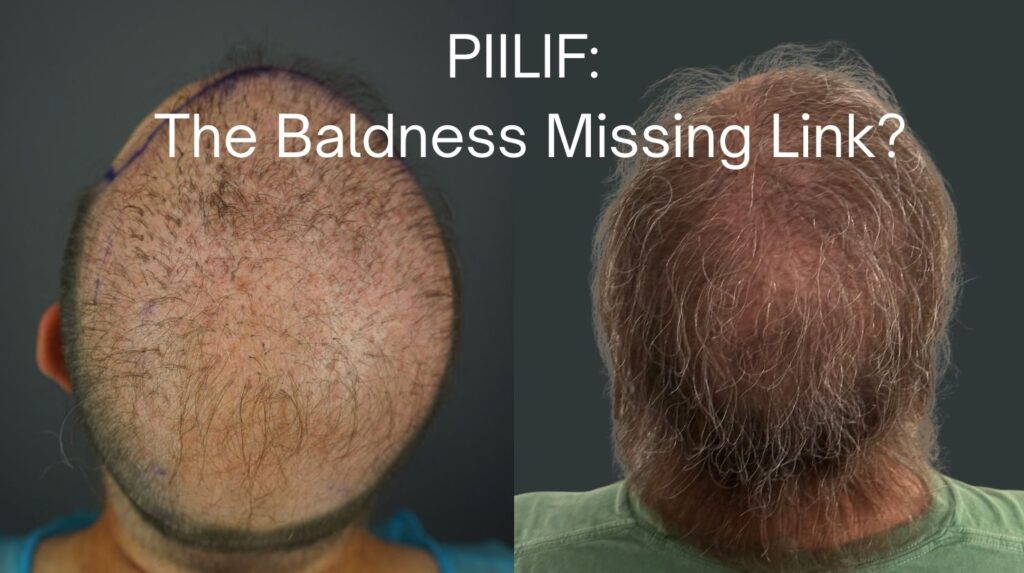
A new publication from Dr. U identifies a subclinical inflammatory and early fibrotic scalp pattern that can coexist with androgenetic alopecia, influence outcomes, and change how we plan treatment and hair restoration for hair loss and pattern baldness.
If this sounds like you, this article is for you:
- You are consistent with treatment, but your hair loss or baldness still progresses.
- Minoxidil and/or finasteride helped at first, then results slowed or stopped.
- You have “dandruff” or scalp irritation that keeps coming back.
- A hair transplant result was disappointing, unpredictable, or did not last.
If you are doing “all the right things” for your androgenetic alopecia or pattern baldness, but results are stalling, read this.

Androgenetic alopecia (AGA), also known as male pattern baldness (MPB) or female pattern hair loss (FPHL), is common, visible, and emotionally heavy. Many patients do everything they are told: minoxidil, finasteride (or dutasteride), devices, shampoos, supplements, and still find that progress slows, stops, or becomes unpredictable.
When that happens, it is not always “bad luck,” and it is not always “you waited too long.”
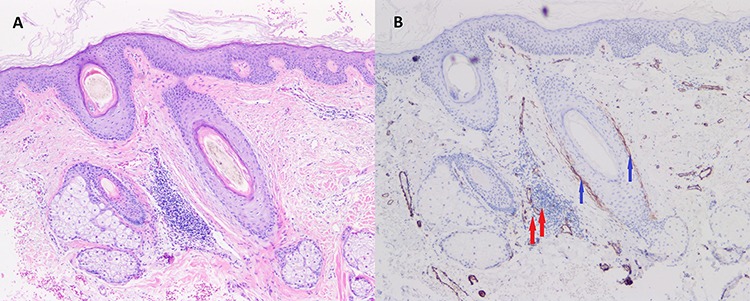
The study titled “Perifollicular Inflammation and Fibrosis in Androgenetic Alopecia: Implications for Diagnosis and Treatment – A Comparative Histopathologic and Clinical Study with Normal-Appearing Scalp” was published in the peer-reviewed Clinical Cosmetic and Investigational Dermatology journal. There, we describe a specific histologic pattern that can live quietly under the surface and help explain why some AGA and pattern baldness patients stop responding as expected, progress faster, or respond unpredictably to both medical therapy and hair restoration surgery.
It is called PIILIF, short for Perifollicular Infundibulo-Isthmic Lymphocytic Infiltrates and Fibrosis.
Quick takeaways
- PIILIF is a low-grade, immune-type inflammatory and early fibrotic pattern found around the upper portion of hair follicles (infundibulo-isthmic region) that can coexist with AGA and pattern baldness.
- It can be easy to miss clinically and can be mislabeled as “seb derm” or “just dandruff.”
- It may help explain why finasteride or minoxidil alone may not be enough for some people over time.
- It supports a dual-pathway strategy: address the hormonal pathway and the immune-fibrotic pathway, not one or the other.
- This is exactly why I created the Inflammatory AGA Screen Program (PIILIF Track).
- Important classification insight: the paper proposes that what has been described as fibrosing alopecia of patterned distribution (FAPD) aligns with a later stage of AGA-PIILIF, and recommends staging AGA-PIILIF by the degree of perifollicular fibrosis to support earlier recognition and intervention.
The missing link for AGA medication non-responders
This section is for the patient who is not planning surgery (or not yet), but is frustrated because the standard plan is not delivering what it should.
If the scalp environment is immunologically active and early fibrosis is already present, “more of the same AGA routine” is not always the answer.
The answer is:
- better biology control
- better targeting
- better timing
Here is the practical point
If PIILIF is present, “DHT control only” can leave a second driver running.
Standard AGA treatment often focuses on androgen signaling and follicle cycling support (for example, finasteride and minoxidil). That can be appropriate, but in a subset of patients, there is an additional layer: a perifollicular inflammatory and early fibrotic process that may continue even when DHT is addressed.
That is why some patients report:
- good early improvement, then slow decline again
- a stable period, then sudden acceleration
- “I’m consistent, but the response does not match the effort”
What this changes in real life
For the non-responder, the best move is not to guess harder.
It is to confirm what is actually happening in the scalp environment, and then treat the relevant pathways when indicated.
That does not mean every patient needs a biopsy.
It means:
- for non-responders, ambiguous cases, or high-stakes decisions, it is worth considering early diagnostic confirmation, not late.
What is PIILIF, in plain language?
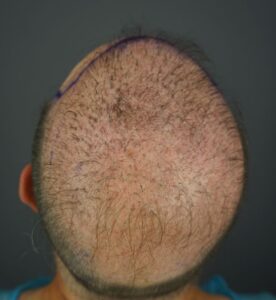
PIILIF describes a subclinical perifollicular inflammatory pattern that concentrates around the upper follicle and is associated with early perifollicular fibrosis.
Key idea: it can be present even when the scalp looks “quiet,” and it can be present even in areas that are not yet visibly thinning or bald.
This matters because once fibrosis progresses, it can reduce the predictability of regrowth and restoration. That is why early recognition is the whole game.
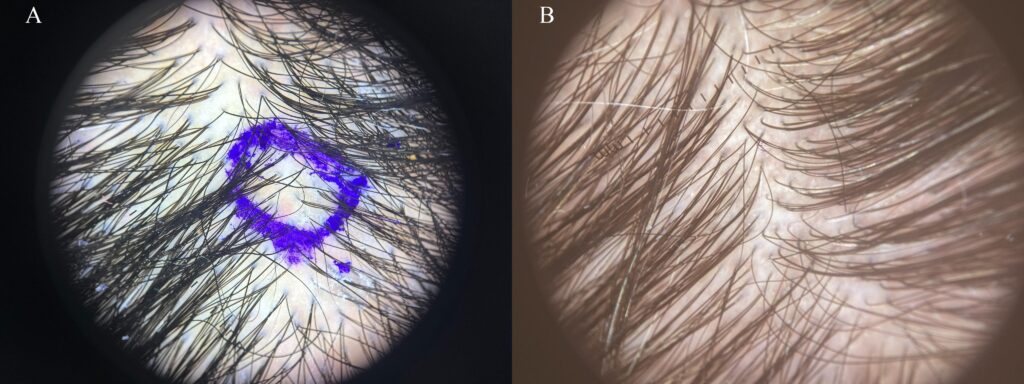
Seeing PIILIF makes the concept clearer.
The short video below illustrates how PIILIF can exist beneath visible pattern baldness and why scalp biology matters when treatments or hair transplants stop responding.
Where FAPD fits: why this paper matters beyond “routine AGA”
If you have heard the term FAPD (fibrosing alopecia of patterned distribution), you already know it sits at the crossroads of two worlds:
- pattern hair loss that looks like AGA or male pattern baldness, and
- fibrosing/scarring biology that behaves more like early scarring alopecia
The key contribution of the paper is that it proposes a unifying framework:
- FAPD may represent a later, more fibrosing stage within the AGA-PIILIF spectrum, rather than a completely separate diagnosis.
- The paper recommends staging AGA-PIILIF by the degree of perifollicular fibrosis, which supports earlier recognition and more informed management decisions.
For patients, the takeaway is not to panic about “scarring.”
The takeaway is precision: if inflammatory and fibrotic drivers are present, it changes what “optimal care” looks like and why durability sometimes requires more than growth stimulation alone.
Why PIILIF gets mislabeled as seb derm or “just dandruff”
Many people with PIILIF report flaking, scale, or irritation. So it is easy to default to seborrheic dermatitis (“seb derm”) or “dandruff.” Whatsmore, the trichoscopic features of PIILIF may show similar findings associated with seborrheic dermatitis
But in our cohort, true seborrheic dermatitis on biopsy was rare compared with PIILIF.
Even when anti-dandruff shampoos temporarily improve scale or redness, that does not necessarily address the deeper perifollicular inflammatory process.
If you are treating “seb derm” aggressively and hair outcomes are still slipping, it is time to consider whether the label is wrong.
Why this matters for hair transplant planning
If the scalp environment is immunologically active and early fibrosis is already present, “more grafts” is not the answer.
The answer is:
- better biology control
- better planning
- better timing
In higher-risk candidates, pre-transplant control of PIILIF and biopsy-informed planning are advisable.

That does not mean every patient needs a biopsy. It means that for non-responders and high-stakes surgical candidates, diagnostic confirmation should be considered early rather than late.
Who should consider PIILIF screening?
You should at least consider PIILIF screening if you relate to one or more of these:
- You are not responding as expected to a well-run AGA regimen (meds, topical plan, lifestyle, compliance is solid).
- You have been told you have “seb derm” for years, but hair continues to miniaturize.
- You have advanced AGA or you are a complex case (including prior surgery, donor depletion, body hair follicular unit excision (FUE) or beard hair FUE reliance).
- You are planning a transplant and you want to reduce the risk of disappointing yield, ongoing thinning, or unpredictable healing.
- You are 44 years or older.
- You have perifollicular scale, redness, itch, tenderness, or shedding that does not match the clinical look of “routine AGA.”
- You developed overt features of scarring alopecia or severe inflammation after a hair transplant.
The Inflammatory AGA Screen Program (PIILIF Track)
I created this because too many complex patients with hair loss and baldness were being managed with a one-pathway playbook.
Program name: Inflammatory AGA Screen Program (PIILIF Track)
Format: Virtual first (with in-person follow up when needed)
Deposit: Required to protect quality, reduce no-shows, and allow proper time allocation
What the PIILIF Track helps us do
- Identify whether a patient’s AGA is likely “standard AGA” alone, or AGA plus PIILIF biology.
- Decide when a biopsy is appropriate and where it should be taken to improve diagnostic yield.
- Build a personalized plan aimed at:
- controlling the inflammatory axis when indicated
- reducing progression and improving durability
- planning surgery only when the scalp biology is optimized
Long-Term Care Matters Long-term
Sustainable treatment matters because AGA‑PIILIF is a long game
When PIILIF is present, the goal is not a short burst of change. The goal is long-term stability of the scalp environment. PIILIF is best understood as a chronic, genetically influenced tendency toward follicle‑centered inflammation and early fibrosis that is not “cured” once and for all. It is managed. That reality changes how we choose treatments.
Control, not cure, means the plan must be livable for years
If control may need to be maintained for the long term, the foundation of care should be something a patient can realistically sustain. This argues against building the core plan around high‑burden or high‑risk approaches, especially because AGA‑PIILIF can be subtle compared with overt primary scarring alopecias. The biology may be meaningful even when the scalp looks “quiet,” but the management must remain practical and tolerable over time.
What we evaluated in our cohort
Because the working model involves long-term control, the study emphasized steroid-sparing options that may be suitable for longer-term use, with short-course therapies used selectively. Selections were informed by peer-reviewed literature on steroid-sparing management in primary cicatricial alopecias. Treatments used in the cohort, often in combination and individualized to the patient, included:
- Dutasteride and finasteride
- Oral minoxidil
- Topical calcineurin inhibitors
- Minocycline or doxycycline (typically as a time‑limited course)
- A selected phytoactive approach: Gashee topical and Gashee oral
What showed the clearest statistical signal in our analysis (and what did not)
In this retrospective cohort analysis, only some interventions showed a clear statistical association with improvement. In order of p‑value significance, the strongest signals in our dataset were observed with:
- Topical and oral phytoactives (Gashee)
- Topical calcineurin inhibitors
- Minocycline
- Dutasteride
Other treatments used in the cohort (including finasteride, oral minoxidil, and doxycycline) did not show the same level of statistical signal in this dataset. This may reflect sample size, duration, selection bias, combination regimens, dosing, or when and how an agent was deployed, rather than proving a treatment has no role.
The practical takeaway
The point is not that every patient needs every component. The point is that when AGA‑PIILIF biology may require long-term management, the strategy should prioritize approaches that are realistic to sustain, steroid‑sparing when appropriate, and matched to the level of inflammatory and fibrotic activity.
How this relates to Phytoactives
Within a long-term, steroid‑sparing framework, a phytoactive topical or oral option may be considered as supportive care as part of a broader plan, particularly when long‑term tolerability is a priority. In our cohort analysis, the use of Gashee in both topical and oral forms showed the strongest statistical signal among the steroid‑sparing measures evaluated, but this study is observational, and larger studies are needed to confirm and refine these findings. Gashee is not a substitute for diagnosis and is not positioned as a cure. It may be one tool within a clinician‑guided program when it fits the patient’s overall plan and risk profile.
Where a phytoactive product like Gashee fits (and where it does not)
Important points of clarification.
What Gashee is not
- It is not positioned as a “cure” for AGA, hair loss, or baldness.
- It is not a replacement for diagnosis.
- It is not a substitute for physician-directed therapy when stronger interventions are warranted.
Where Gashee can fit logically in the PIILIF conversation
PIILIF changes the strategy from “only push growth” to “optimize the scalp environment and protect follicle viability.”
Because AGA is a long-course condition, and because PIILIF (when present) can behave like a persistent, low-grade inflammatory process, long-term tolerability matters. That pushes smart clinicians toward steroid-sparing approaches whenever feasible.
In our PIILIF work, the practical takeaway is that some patients benefit when care includes scarring alopecia or PCA (primary cicatricial alopecia)-style anti-inflammatory and anti-fibrotic measures alongside appropriate androgen management.
In that context, phytoactive support can be part of a long-term maintenance philosophy, particularly for patients who need a plan they can sustain.
Gashee exists in both topical and oral forms. In my practice, when it is used, it is used as part of a broader plan, not as a standalone promise.
Important note: Gashee is designed to support the scalp environment as part of a broader hair loss program. It is not intended to diagnose, treat, cure, or prevent disease. Individual results vary.
The bigger point: stop guessing. Start staging.
If the biology is wrong, the plan will be wrong.
PIILIF gives us a clearer framework for:
- earlier detection
- better durability
- better surgical planning
- fewer “mystery non-responders”
If you are a patient who feels stuck, or a clinician managing difficult AGA cases, the PIILIF Track is built for you.
Next steps
Patients: Request a PIILIF Track evaluation
Start the PIILIF Track Intake
Clinicians: Refer a complex AGA case for PIILIF screening
Clinician Referral: PIILIF Track
Medical and product disclaimer
- Gashee is designed to support the scalp environment as part of a broader hair loss program. It is not intended to diagnose, treat, cure, or prevent disease.
- This article is for educational purposes and does not provide medical advice. Diagnosis and treatment should be individualized and guided by a qualified clinician. Product statements have not been evaluated by the FDA. Products are not intended to diagnose, treat, cure, or prevent any disease.
FREQUENTLY ASKED QUESTIONS
PIILIF, FAPD, treatment resistance, and what to do next
1) What is PIILIF?
PIILIF stands for Perifollicular Infundibulo-Isthmic Lymphocytic Infiltrates and Fibrosis. In plain terms, it describes a low-grade immune-type inflammation and early fibrotic change occurring around the upper portion of the hair follicle. It can coexist with androgenetic alopecia (AGA), also known as male pattern baldness or female pattern hair loss, and may be present even when the scalp looks “normal” on casual inspection.
2) Is PIILIF the same as FAPD?
Not exactly. FAPD (fibrosing alopecia of patterned distribution) is a term typically used when patterned hair loss shows a more advanced fibrosing or scarring-leaning biology. The key insight from this publication is that FAPD may align with a later stage within an AGA-PIILIF spectrum, rather than representing a completely separate condition.
From a practical standpoint, this means that earlier recognition of inflammatory and fibrotic drivers matters. Identifying AGA-PIILIF before extensive fibrosis develops allows clinicians to plan care with durability in mind, when the biology may still be more modifiable.
Waiting until the histologic features associated with FAPD are fully established may correspond to a more treatment-resistant stage. For this reason, the authors emphasize the value of recognizing and addressing AGA-PIILIF earlier, rather than deferring evaluation until later stages when fibrotic changes are more entrenched.
3) Do I need a biopsy to know if I have PIILIF?
Not everyone needs a biopsy. A biopsy becomes more relevant when your provider finds signs of inflammation on magnified (trichoscopic) examination of your scalp. The threshold is reduced if you are already a non-responder, your presentation is ambiguous, you have symptoms that do not fit “routine AGA” (itch, tenderness, burning, persistent scale), or you are making high-stakes decisions like hair transplant planning. The goal is not to biopsy everyone, it is to confirm scalp biology early when the stakes or uncertainty are high.
4) Why did my finasteride or minoxidil stop working?
There are several reasons treatments may stop working, and not all are about the medication itself. The main concept here is that AGA or pattern baldness is often treated as purely androgen-driven, but in a meaningful subset of patients an inflammatory and early fibrotic process may be operating in parallel. If that second driver is active, “more DHT control” alone may not fully stabilize the situation, which is why biology-aware evaluation and a dual-pathway strategy may be needed in selected cases.
5) Can PIILIF affect hair transplant outcomes?
It can. Hair transplantation is not just about graft numbers or technique, it is also about the health of the recipient scalp environment and long-term stability of surrounding native hair. If inflammatory-pattern biology and early fibrosis are active, predictability and durability can be affected, which is why scalp optimization and biopsy-informed planning can be important in higher-risk candidates.
6) What are phytoactives, and where do they fit in a long-term plan?
Phytoactives are plant-derived compounds that may support the scalp environment as part of a broader hair loss program. In a long-term maintenance context, many patients and clinicians prefer steroid-sparing approaches when appropriate, especially when scalp inflammation behaves as a chronic, low-grade process. In that framework, a phytoactive topical or oral product can be considered as supportive care, but it is not a replacement for diagnosis, and it should be used as part of a clinician-guided plan when stronger interventions are indicated.
7) Does PIILIF require lifelong treatment?
PIILIF, when present, may behave like a chronic, genetically influenced inflammatory tendency around hair follicles. The practical goal is long-term control and stability, not a one-time cure. Some patients may need ongoing maintenance for years, with the plan adjusted over time based on symptoms, exam findings, and overall risk profile under clinician guidance.
8) Do I need strong steroids or immunosuppressants to control PIILIF?
Not necessarily. AGA-PIILIF can be subtle compared with overt primary scarring alopecias, so aggressive therapy is not automatically the default. In our cohort, the emphasis was on steroid-sparing strategies that can be considered for longer-term use when clinically appropriate. Treatment choice and intensity should be individualized and supervised by a qualified clinician.
9) What kinds of long-term, steroid-sparing treatments were used in the study?
In this cohort, patients were managed with a steroid-sparing approach tailored to clinical context and often used in combination. Treatments used included dutasteride or finasteride, oral minoxidil, topical calcineurin inhibitors, and time-limited tetracyclines (such as minocycline or doxycycline). A selected phytoactive topical and oral option (Gashee) was also used as part of the broader scalp-care plan when appropriate.
In this retrospective dataset, the clearest statistical associations with improvement were observed in regimens that included: Gashee topical, Gashee oral, topical calcineurin inhibitors, minocycline, and dutasteride. Because many patients received combination regimens, these findings do not establish that any single component alone caused the observed outcomes. Observational findings do not prove cause and effect, larger studies are needed, and individual results vary. Gashee is not intended to diagnose, treat, cure, or prevent disease.
Important note: Products and supplements are not intended to diagnose, treat, cure, or prevent disease. Individual results vary, and medical decisions should be individualized with a qualified clinician.